"When you reach the end of your rope, tie a knot in it and hang on." ~Thomas Jefferson
A lot has happened since my last post, and I have no idea where to start. It's as though I was a hostage in the months of September and October, and I've just wanted to rewind time and go back to August. Life isn't like that though, there is no going back...just forward.
In September, when my intravenous antibiotics were switched to Merropenem and Colistin, I started to feel different. My O2 had dropped from a 98% to 93% pulse oxygen rate since the bronchoscopy and port was placed, but I had thought it would be temporary and that it would come back if I just gave my body some time to fight infection and recover. As days went by, I was experiencing high tachycardia (increased heart rate) and my O2 started dropping to the 80's on room air. I wasn't able to breath on my own without the help of oxygen. My doctor ordered a CT scan of my lungs with contrast. When the contrast was pumped into my heart, I had my eyes closed. I saw an orange flash and I felt a warm sensation in my chest. My O2 dropped to 70 and I was rushed to the E.R. I was so glad to have my friend Paula there because this was not the norm for me and I was scared.
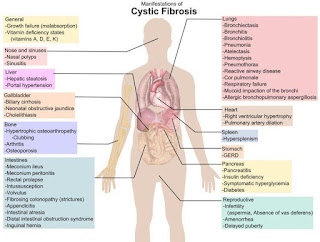
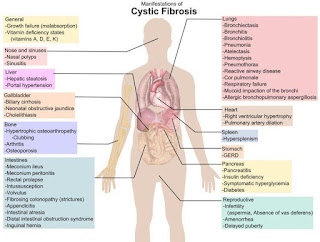
I knew that the reason why my oxygen dropped to 70% was from the reaction to the contrast. But what was causing my O2 to be in the 80's before that was the big question. A part of me wanted to put all the blame on the port because of the fact that it was a new, unfamiliar, foreign object in my body. I wondered if my body was rejecting it and if my sudden symptoms could easily be fixed by taking the thing out. Then, I wondered if it could be a reaction to the toxic intravenous medications that were being pumped into my heart. And my final guess was simply Cystic Fibrosis, the culprit that I fight so hard every day to just keep jailed up.
I know that when living with Cystic Fibrosis, life can change in an instant. I'm not oblivious to what the disease can do. I have heard stories of those who have lost their battle with Cystic Fibrosis. The cause of death in a Cystic Fibrosis patient is usually respiratory tract infections, respiratory distress, transplant rejection, or complications from Cystic Fibrosis. Though, I want my story to be different - I want to somehow change my story. That is why I fight so hard everyday to defeat Cystic Fibrosis, the disease that tries to rob me, hold me back, and steal everything away.
Dr. Layish (my Orlando doctor) did not have any answers. After 3 weeks of intravenous antibiotics, the Merrepenem seemed like the culprit and I was taken off of the antibiotics. My O2 was sitting stable at 92% in the hospital, so I got the go-ahead to be released. I was off intravenous antibiotics for a week to try to see if that would make everything better. I know it might sound crazy, but I decided to go to New York with my mom for four days. It was a mother/daughter vacation that we had always wanted to go on. I did not want my Cystic Fibrosis to steal that away from me, and I thought to myself, as they say on broadway: the show must go on! It was an amazing four days with my mom. I made sure to have oxygen there when I arrived so that if my symptoms were to occur again, I would have backup. And I made sure to sleep with the oxygen at night as well. On the airplane ride back, my lips and fingernails suddenly turned blue, which had never happened to me before. The stewardess grabbed a tank of oxygen to help me breathe. I was scared. My body was giving me clues that something was wrong.
My oxygen was constantly fluctuating. One moment I would be fine at 92%, and the next, I would be needing oxygen to breathe. My doctor ordered a bag pack and small oxygen tanks for me to carry with me during the day. He did not seem to have any answers. In fact, he actually asked ME what I wanted HIM to do. I was in shock! Isn't he supposed to be the doctor? Dr. Layish always sends me to an infectious disease doctor when it is time for I.V.'s, and even though I am not contagious, he feels that she is the best person to decide which intravenous medications should be used to treat my infections. Usually, a good Cystic Fibrosis doctor knows everything there is to know about Cystic Fibrosis, especially when it comes to treating infections with intravenous antibiotics. This goes to show that he truly doesn't have a clue. Dr. Curbelo, my infectious disease doctor, decided more intravenous antibiotics were necessary, and that the cause of all this commotion was not the port, but rather my Cystic Fibrosis. I started back on intravenous antibiotics on October 11th.
Colistin (every 12 hrs) and Cefepime (every 8 hrs)...only to find out one week later that I wasn't getting any better, due to the fact that I was resistant to the Cefepime.
My antibiotics were then changed to Colistin (every 12 hours) and Azactam (every 8 hrs), on October 17th, and I have remained on these drugs since then.
I have finally decided that it is time for a change. Enough is enough. Time for a new CF doctor. My best friend, Christina, is amazing! She drove me down to Palm Beach to help me find answers. She was my old college roommate and has been through it all with me. I have heard many great things about Dr. Salathe, and I decided after we met that I wanted him to be my new doctor. When I lived in Miami last year, Dr. Light was my Cystic Fibrosis doctor. When I told him that I was moving back to Orlando, he informed me that he was retiring and that I could always drive to Palm Beach to see Dr. Salathe, but I felt that the drive was just too far. For the sake of convenience, I told myself that my old Orlando doctor would do fine, but who am I kidding? Cystic Fibrosis doctors in Miami are simply the best in Florida. And if I want to get the best treatment, I need to make the 3-hour drive for it. I think it will be worth it. Dr. Salathe wants to start from scratch and reevaluate my overall condition. Tomorrow morning, Hunter is taking me to the hospital in Miami. Dr. Salathe's game plan for me includes vigorous chest physiotherapy, prolonged intravenous antibiotics, around the clock inhaled medications, and generally kicking some CF butt!
I'm aware that I have holes in my lungs from the disease, and mucus galore blocking my airways, but it's like I said - I want my story to be different. I want a doctor that will also be my cheerleader. I don't want to be a statistic. I want someone that will fight as hard as me to keep me going. At times, I think my mind has gotten me this far. The constant push to survive; the will to beat the odds. September and October might have been stolen from me, but I want to enjoy my November and, more importantly, my 27th birthday in December.